
gerd diet plan menu pdf free download
GERD is a chronic condition where stomach acid flows back into the esophagus, causing heartburn and discomfort. Diet plays a crucial role in managing symptoms, as certain foods can trigger or alleviate acid reflux. By focusing on low-acid, high-fiber, and anti-inflammatory foods, individuals can reduce discomfort and improve digestive health.
1.1 What is GERD?
GERD, or Gastroesophageal Reflux Disease, is a chronic digestive disorder where stomach acid frequently flows back into the esophagus, causing irritation and discomfort. This condition occurs when the lower esophageal sphincter (LES), a muscle that separates the esophagus and stomach, fails to close properly or weakens over time. As a result, acid reflux becomes a recurring issue, often leading to symptoms like heartburn, chest pain, and difficulty swallowing. GERD is typically diagnosed when these symptoms occur at least twice a week, significantly impacting daily life and overall health. Understanding GERD is essential for implementing an effective diet plan to manage its symptoms and improve quality of life.
1.2 Symptoms of GERD
GERD symptoms vary in severity and frequency but often include heartburn, a burning sensation in the chest and throat, especially after eating or lying down. Regurgitation of food or sour liquid is common, along with difficulty swallowing (dysphagia) and chest pain that may mimic heart attack symptoms. Some individuals experience coughing, hoarseness, or a sore throat due to acid reflux reaching the upper airway. Less frequently, GERD can cause bad breath, dental erosion, or a sensation of food getting stuck in the throat. Persistent or severe symptoms warrant medical attention, as untreated GERD can lead to complications like esophageal damage or narrowing. Recognizing these symptoms is crucial for early diagnosis and effective management.
1.3 The Role of Diet in Managing GERD
Diet plays a pivotal role in managing GERD, as certain foods can trigger or alleviate symptoms. Acidic foods like citrus fruits, tomatoes, and chocolate, as well as caffeinated beverages, alcohol, and spicy dishes, often exacerbate heartburn. By avoiding these triggers and incorporating low-acid, high-fiber, and anti-inflammatory foods, individuals can reduce acid reflux. Alkaline foods, such as bananas, melons, and green vegetables, help neutralize stomach acid, while lean proteins and whole grains support digestive health. Portion control and eating smaller, more frequent meals also ease pressure on the lower esophageal sphincter. A tailored GERD diet plan can significantly improve symptoms and overall well-being, making it a cornerstone of disease management.

Benefits of a GERD Diet Plan
A GERD diet plan helps reduce acid reflux symptoms, improves digestion, and offers long-term health benefits by promoting a balanced and nutrient-rich eating approach.
2.1 Reducing Acid Reflux Symptoms
A GERD diet plan focuses on minimizing foods that trigger acid reflux, such as citrus fruits, tomatoes, chocolate, and fatty or fried items. By incorporating alkaline foods like bananas, melons, and leafy greens, individuals can help neutralize stomach acid and reduce esophageal irritation. Additionally, avoiding large meals and opting for smaller, more frequent ones prevents excessive pressure on the lower esophageal sphincter, which can lead to reflux episodes. This structured approach not only alleviates heartburn and discomfort but also creates a foundation for sustainable symptom management. Regular adherence to such a diet can significantly improve quality of life for those with GERD.
2.2 Promoting Digestive Health
A GERD diet plan emphasizes foods that support overall digestive well-being, reducing inflammation and enhancing gut function. High-fiber options like whole grains, vegetables, and legumes promote regular bowel movements and prevent constipation. Lean proteins, such as poultry and fish, aid in maintaining muscle strength without overburdening the digestive system. Incorporating healthy fats, such as avocado and olive oil, supports nutrient absorption and soothes the esophageal lining. Staying hydrated is also crucial, as water helps dilute stomach acid and facilitate digestion. By focusing on balanced, nutrient-rich meals, individuals can foster a healthier digestive system, reducing the likelihood of acid reflux episodes and improving long-term digestive health. Portion control and mindful eating further enhance these benefits.
2.3 Long-Term Health Benefits
Adopting a GERD-friendly diet offers numerous long-term health benefits beyond symptom relief. By focusing on nutrient-rich, low-acid foods, individuals can reduce chronic inflammation, which is linked to conditions like heart disease and diabetes. A balanced diet also promotes sustainable weight management, which is crucial for reducing pressure on the lower esophageal sphincter. Over time, this can lead to improved overall health and a lower risk of complications associated with untreated GERD, such as esophageal damage. Additionally, a diet rich in fiber and antioxidants supports better nutrient absorption and may enhance energy levels. By committing to a GERD diet plan, individuals can achieve long-term digestive and systemic health benefits, improving their quality of life.

Core Components of a GERD Diet Plan
A GERD diet plan focuses on balancing foods that reduce acid reflux and promote digestive health. It emphasizes low-acid meals, high-fiber intake, and portion control to minimize symptoms.
3.1 Foods to Eat
Incorporating the right foods into your GERD diet is essential for managing symptoms. Focus on alkaline foods like bananas, melons, and green vegetables, which help neutralize stomach acid. Anti-inflammatory options such as ginger, chamomile tea, and whole grains can reduce irritation. High-fiber foods like whole grains, beans, and apples support digestive health and prevent reflux. Lean proteins, including poultry, fish, and tofu, are ideal for balanced meals. Healthy fats like avocado, olive oil, and nuts are also beneficial. These foods promote healing, reduce inflammation, and create a protective barrier against acid reflux. By prioritizing these options, you can alleviate symptoms and improve overall well-being.
3.2 Foods to Avoid
Identifying and avoiding trigger foods is crucial for managing GERD. Foods that are high in acid, such as citrus fruits, tomatoes, and vinegar-based products, can exacerbate symptoms. Fried and fatty foods, including red meat and processed snacks, slow digestion and relax the lower esophageal sphincter, leading to reflux. Spicy dishes, chocolate, and caffeine can also irritate the esophagus and worsen heartburn. Additionally, carbonated beverages like soda and alcohol can increase stomach pressure, promoting acid reflux. By eliminating these foods from your diet, you can significantly reduce GERD symptoms and improve your quality of life. A structured meal plan can help you avoid these triggers effectively.
3.3 Meal Frequency and Portion Control
Eating smaller, more frequent meals throughout the day can help manage GERD symptoms by reducing stomach pressure and preventing acid reflux. Opt for 4-6 smaller meals instead of three large ones to avoid overloading the stomach. Portion control is key—avoid overeating, as this can strain the lower esophageal sphincter (LES). Use smaller plates to help manage serving sizes. Additionally, avoid lying down for at least 2-3 hours after eating to allow proper digestion. Drinking water between meals rather than during meals can also reduce bloating. Chewing food thoroughly and eating slowly further aids digestion and minimizes discomfort. This approach ensures a balanced and comfortable eating pattern, essential for GERD management.

7-Day GERD Diet Plan Overview
This structured plan provides daily meal ideas to alleviate GERD symptoms. It includes breakfast, lunch, dinner, and snacks, focusing on low-acid and anti-inflammatory foods for optimal relief and digestive health.
Day 1 focuses on introducing meals that are gentle on the esophagus and reduce acid reflux. Start with oatmeal for breakfast, paired with low-acid fruits like bananas or melons. For lunch, opt for grilled chicken or fish with steamed vegetables like green beans or carrots. Dinner could include lean turkey or tofu with quinoa and sautéed spinach. Snacks such as almonds or cucumber slices are ideal. Avoid spicy, fatty, or citrus-based foods. This day sets the foundation for a GERD-friendly diet, emphasizing small, frequent meals to ease digestion and minimize stomach pressure.
4.2 Day 2: Incorporating Alkaline Foods
Day 2 introduces alkaline-rich foods to help neutralize stomach acid and reduce irritation. Begin with a breakfast of scrambled eggs with spinach and whole-grain toast. For lunch, enjoy a salad with grilled chicken, cucumber, and bell peppers, dressed with olive oil and herbs. Dinner features baked cod with steamed asparagus and brown rice. Snacks include fresh melon slices or a small handful of almonds. Alkaline foods like vegetables, lean proteins, and whole grains are prioritized to create a balanced and soothing menu. This day emphasizes the role of pH-neutral foods in calming GERD symptoms and promoting digestive comfort.
4.3 Day 3: Anti-Inflammatory Food Options
Day 3 focuses on anti-inflammatory foods to reduce esophageal irritation and alleviate GERD symptoms. Start with oatmeal topped with sliced bananas and a sprinkle of cinnamon for breakfast. Lunch features a grilled turkey and avocado wrap with mixed greens, using a whole-grain tortilla. Dinner includes baked salmon, roasted sweet potatoes, and steamed broccoli. Snacks like apple slices with almond butter or a small handful of walnuts are ideal. Anti-inflammatory foods such as ginger, chamomile tea, and omega-3-rich fish help soothe the digestive tract and minimize inflammation. This day’s menu emphasizes nutrient-dense options to promote healing and long-term symptom relief.
4.4 Day 4: Low-Acid Meal Ideas
Day 4 focuses on low-acid meals to minimize acid reflux triggers. Breakfast includes scrambled eggs with spinach, whole-grain toast, and a side of sliced melon. For lunch, enjoy a grilled skinless chicken breast with quinoa and steamed green beans. Dinner features baked cod with roasted carrots and brown rice. Snacks include rice cakes with a drizzle of honey or sliced cucumbers. These meals avoid high-acid ingredients like citrus or tomatoes, reducing irritation to the esophagus. Low-acid foods help maintain a balanced stomach pH, alleviating heartburn and promoting a comfortable digestive experience throughout the day.
4.5 Day 5: High-Fiber Foods for Digestive Health
Day 5 emphasizes high-fiber foods to support digestive health and reduce GERD symptoms. Breakfast includes oatmeal with sliced bananas, a handful of berries, and a sprinkle of almond butter. Lunch features a mixed green salad with grilled chicken, cucumber, and a light vinaigrette, paired with a whole-grain wrap. Dinner consists of baked chicken breast with roasted Brussels sprouts and sweet potatoes. Snacks include apple slices with a small portion of peanut butter or celery sticks with hummus. High-fiber foods aid in digestion, reduce pressure on the lower esophageal sphincter, and promote regular bowel movements, helping to alleviate acid reflux discomfort. Portion control and hydration are key to maximizing benefits.
4.6 Day 6: Avoiding Trigger Foods
Day 6 focuses on eliminating trigger foods that can worsen GERD symptoms, such as citrus fruits, tomatoes, chocolate, caffeine, alcohol, and fried or fatty foods. Breakfast includes oatmeal with sliced almonds and a drizzle of honey, avoiding acidic fruits. Lunch features a grilled chicken salad with mixed greens, cucumbers, and carrots, dressed with olive oil and herbs. Dinner consists of baked fish with steamed green beans and quinoa. Snacks include small portions of raw vegetables like celery or bell peppers. By avoiding trigger foods, individuals can reduce acid reflux episodes and promote a healing environment for the esophagus. Portion control and hydration remain essential for optimal benefits.
4.7 Day 7: Sustaining GERD Diet Progress
Day 7 emphasizes maintaining long-term adherence to the GERD diet plan. Breakfast includes oatmeal with sliced bananas and a sprinkle of cinnamon, avoiding acidic fruits. Lunch features a lean turkey and avocado wrap with whole-grain tortillas and a side of mixed greens. Dinner consists of grilled salmon, steamed asparagus, and quinoa. Snacks include small portions of rice cakes with almond butter or baby carrots. This final day reinforces the importance of portion control, hydration, and avoiding late-night eating. By incorporating these habits, individuals can sustain progress, reduce symptoms, and promote overall digestive health. Continued monitoring of symptoms and adjustments to the plan ensure long-term success.

Tips for Managing GERD Symptoms
- Lifestyle changes, such as regular physical activity, can help alleviate GERD symptoms.
- Avoid eating close to bedtime to reduce nighttime acid reflux.
- Eat smaller, more frequent meals to prevent stomach distension.
- Track triggers and symptoms using a daily diary for better management.
- Consistency in following the GERD diet plan is key to long-term relief.
5.1 Lifestyle Changes Beyond Diet
Adopting lifestyle changes beyond diet is essential for managing GERD symptoms effectively. Regular physical activity, such as walking or yoga, can improve digestion and reduce acid reflux. Maintaining a healthy weight helps alleviate pressure on the stomach, which can contribute to GERD. Avoiding tight clothing and avoiding smoking or alcohol consumption are also beneficial. Elevating the head of your bed by 6-8 inches during sleep can prevent nighttime acid reflux. Additionally, avoiding late-night eating and minimizing portion sizes can further reduce symptoms. Staying hydrated and managing stress through relaxation techniques like deep breathing or meditation can also support overall digestive health. These changes, combined with a GERD-friendly diet, promote long-term symptom relief and improved well-being.
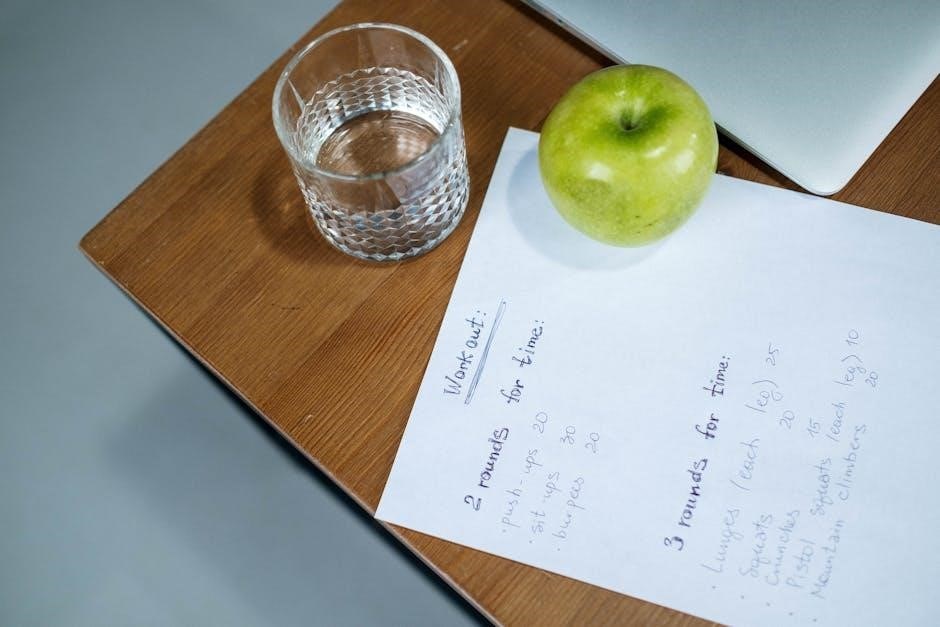
5.2 Importance of Regular Physical Activity
Regular physical activity plays a significant role in managing GERD symptoms. Exercise helps maintain a healthy weight, reducing pressure on the stomach that can trigger acid reflux. Activities like walking, yoga, or swimming improve digestion and strengthen abdominal muscles, which can help prevent reflux. Even moderate exercise, such as light stretching or brisk walking, can lower GERD symptoms by promoting better stomach emptying. However, avoid vigorous workouts immediately after meals, as this can worsen reflux. Incorporating physical activity into your daily routine, combined with a GERD-friendly diet, can enhance overall well-being and provide long-term relief from acid reflux symptoms.
5.3 Avoiding Late-Night Eating
Avoiding late-night eating is crucial for managing GERD symptoms. Lying down immediately after meals can cause stomach acid to flow back into the esophagus, worsening heartburn. Finish eating at least 2-3 hours before bedtime to allow digestion to begin. Heavy or rich meals in the evening are particularly problematic, as they can delay digestion and increase reflux risk. Opt for light, GERD-friendly snacks if needed, and avoid trigger foods like chocolate, citrus, or fatty foods. Raising the head of the bed by 6-8 inches can also help prevent nighttime reflux. Combining this practice with a balanced GERD diet plan enhances symptom relief and improves overall digestive comfort.

Downloading the Free GERD Diet Plan PDF
Access a free GERD diet plan PDF online. This guide offers meal ideas and tips to manage acid reflux symptoms effectively through dietary changes.

6.1 Steps to Access the PDF Guide
To download the free GERD diet plan PDF, visit the provided link and click the “Download” button. Enter your email address if prompted to receive the guide. Open the PDF to explore a detailed 7-day meal plan, complete with breakfast, lunch, dinner, and snack options. The guide includes low-acid, anti-inflammatory, and high-fiber foods to alleviate symptoms. Print the document for easy meal prep and tracking. Use the included templates to customize your diet plan based on preferences and needs. This resource is designed to help you manage GERD effectively and sustainably, ensuring a clear path to reducing acid reflux and improving digestive health.
6.2 Customizing the Diet Plan
The GERD diet plan PDF allows for customization to suit individual preferences and needs. Users can adjust portion sizes, swap ingredients, and incorporate personal favorites while adhering to the low-acid, high-fiber framework. Tracking progress with a symptom diary helps identify trigger foods and monitor improvements. For those with severe symptoms or additional health conditions, consulting a healthcare provider or dietitian can provide further tailored guidance. This flexibility ensures the diet remains sustainable and effective, empowering individuals to take control of their GERD management while enjoying meals that align with their lifestyle and dietary goals.
Adopting a GERD-friendly diet can significantly alleviate symptoms and improve quality of life. Start your journey with the provided 7-day plan and track your progress for lasting relief.
7.1 Summary of Key Takeaways
Managing GERD through diet is essential for symptom relief. Focus on low-acid, high-fiber foods, and avoid triggers like citrus fruits and fatty meals. Incorporate alkaline and anti-inflammatory options to reduce discomfort. Smaller, frequent meals can ease digestion, while avoiding late-night eating prevents reflux. Tracking symptoms and progress helps tailor the diet plan. Regular physical activity supports overall digestive health. Customize the 7-day GERD diet plan to suit personal preferences and needs. Consistency and patience are key to achieving long-term benefits and improving quality of life. Refer to the provided resources for additional guidance and support.
7.2 Encouragement to Start the Diet Plan
Starting a GERD diet plan is a proactive step toward alleviating symptoms and improving overall well-being. By incorporating the recommended foods and avoiding triggers, individuals can experience significant relief from acid reflux and heartburn. The plan is designed to be flexible and tailored to personal preferences, making it easier to stick with long-term. Consistency is key, as small changes can lead to meaningful improvements in digestive health. Encourage yourself to take the first step today—download the free PDF guide, explore the meal ideas, and begin your journey toward a symptom-free life. Every meal is an opportunity to nourish your body and reduce discomfort.
Additional Resources
Supplement your GERD diet plan with our free downloadable resources, including a comprehensive food list, symptom tracker, and guides for long-term management. These tools empower sustained relief.
8.1 GERD Diet Food List
The GERD diet food list is a comprehensive guide to help manage symptoms by identifying trigger and friendly foods. It categorizes foods into low-acid, high-fiber, and anti-inflammatory options. Alkaline fruits like bananas and melons neutralize stomach acid, while lean proteins and whole grains support digestion. Avoid trigger foods such as citrus fruits, tomatoes, chocolate, and fatty or fried foods. This list empowers individuals to make informed dietary choices, promoting symptom relief and long-term digestive health. Downloadable as a PDF, it serves as a quick reference for meal planning and grocery shopping, ensuring adherence to a GERD-friendly lifestyle. Regular updates keep the information current and relevant.

8;2 Tracking Progress with a Symptom Diary
Tracking progress with a symptom diary is essential for managing GERD effectively. This tool helps identify food triggers, monitor symptom patterns, and evaluate the impact of dietary changes. By documenting meals, portion sizes, and symptom severity, individuals can pinpoint which foods exacerbate reflux. Over time, this data reveals trends, guiding personalized adjustments to the GERD diet plan. Regularly reviewing the diary with a healthcare provider ensures tailored advice and optimal symptom control. Consistency in recording is key to achieving lasting relief and understanding how lifestyle modifications influence digestive health.
8.3 Consulting a Healthcare Professional
Consulting a healthcare professional is crucial for effectively managing GERD. They provide personalized advice based on individual needs and medical history, helping to refine the diet plan for better symptom control. Professionals can monitor progress, adjust recommendations, and address any challenges faced while following the GERD diet. Regular check-ups ensure that the treatment plan is working effectively and allow for timely adjustments. Additionally, healthcare providers can rule out other conditions with similar symptoms and offer guidance on combining dietary changes with medical treatments. Collaborating with a dietitian or gastroenterologist ensures a comprehensive approach to managing GERD and achieving long-term digestive health.
Leave a Reply
You must be logged in to post a comment.